February 16, 2022 | Erin Bluvas, bluvase@sc.edu
Research conducted by investigators at the Rural and Minority Health Research Center has been featured in a special issue on Racism & Health that was published in Health Affairs this month. The study examined spatial access to hospital services for minoritized racial and ethnic groups, concluding that spatial access to hospital services varies across geographic regions in a manner that systematically disadvantages minoritized communities.
Center director and epidemiology associate professor Jan Eberth led the study and was invited to discuss the team’s findings as part of a one-day virtual symposium hosted by Health Affairs to highlight the special issue. The session was attended by government administration officials, members of congress and state health departments, private industry leaders, health care practitioners, patient advocates, consultants, academics and journalists.
“Migration patterns, both voluntary and forced, and territorial acquisitions have resulted in the concentration of minoritized racial and ethnic groups in defined areas,” says Eberth.
The “problem of the color line,” as described by W.E.B. Du Bois in the early 1900s is still present today. Areas with a high density of minoritized racial/ethnic groups, particularly in rural America, consistently face worse access to care than areas with a high density of white residents.
With this study, the researchers focused on structural racism’s impact on disparities in access to a range of healthcare services. They were particularly interested in hospital-based services because of the key role they play in providing care for conditions (e.g., cancer, cardiovascular disease, injuries) that contribute to racial and ethnic disparities in mortality. Further, the trend of hospital closures in rural areas has decreased access to healthcare services even further in the South, where 60 percent of Black Americans live.
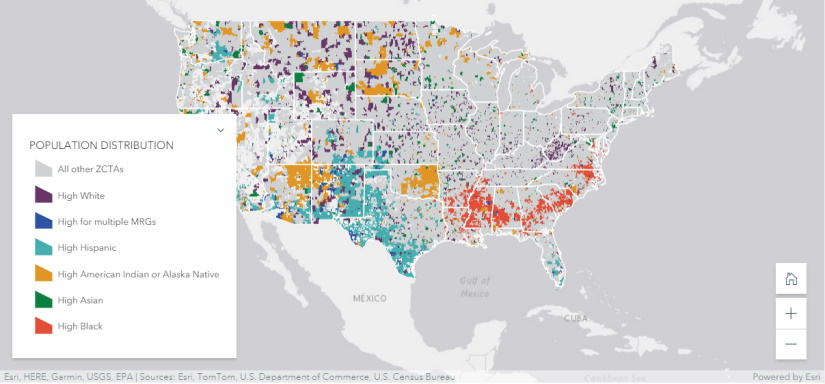
Using data from the American Community Survey, the team used geographic representations of ZIP codes, known as ZIP Code Tabulation Areas (ZCTA), to identify rural and urban areas with the largest representation of minoritized residents. The researchers leveraged data from the American Hospital Association Annual Survey to locate hospital services and then measure the distance between these resources and the ZTCAs.
“High minoritized group ZCTAs are located across the U.S., but we found a clear spatial pattern of Black communities in the South, Hispanic communities in Texas and the West, and American Indian/Alaska Native communities in Oklahoma, the upper Midwest and West,” Eberth says. “Hospital services were closer to high minoritized group ZCTAs in urban areas, but the pattern was reversed in rural areas. Rural high Black and high American Indian/Alaska Native ZCTAs were significantly farther from many hospital services than rural high white areas.”
Their analyses yielded many other findings as well. Results showed variations in access to healthcare services based on type of service, geographic location, population density (rural vs urban), demographics, and other factors. A companion StoryMap was created by the authors and published online alongside the special issue, allowing readers to learn about the historical underpinnings of hospital location decision-making and directly interact with a variety of maps.
The authors note additional challenges in the form of travel barriers, access to facilities that accept a particular insurance (e.g., Medicaid), and specific cultural beliefs/practices.
“When inequalities in the built environment are as large, immobile and capital-intensive as hospitals, approaches to equity must come from multiple directions,” Eberth says. “Policy levers are available at the state and federal levels to address current facility gaps while preventing additional inequities associated with hospital closure or relocation to ensure that future growth reflects community needs.”
Related:
Researchers paint picture of COVID-19 severity, outcomes in South Carolina
Cancer treatment has improved but access to services remains unequal, study finds
Older adults comply with COVID-19 risk mitigation behaviors, but urban-rural disparities persist
Facility ownership matters in the provision of suicide prevention programs, study shows