Being a new or expectant mother can be dangerous, even deadly — even in the U.S. In 2021, more than 1,200 women in the U.S. died during pregnancy or in the six weeks following delivery, a 40 percent increase from the year before. And while the spike can be attributed to the COVID-19 pandemic, the nation’s maternal death rate is still multiple times higher than that of other high-income countries.
Even when inadequate care doesn’t result in death, it can have a lasting impact if women or newborns suffer severe complications, if they don’t receive long-term or follow-up care or if they miss out on critical interventions in the years after childbirth.
But it doesn’t have to be that way. According to the Centers for Disease Control and Prevention, five in six pregnancy-related deaths are preventable; meanwhile, other maternal health risks can be greatly reduced through proper intervention. Across campus, USC’s researchers are on a mission to assist in that effort.
Improving health outcomes through interdisciplinary research
Robin Dail, College of Nursing | Jessica Bradshaw, College of Arts and Sciences
A mother arrives at the delivery room in preterm labor, 12 weeks before her due date. Doctors and nurses are on standby with all the specialized equipment needed to keep the 2-pound baby stable until it can be transported to a NICU or a larger hospital. Among that equipment is something unexpected. As soon as the baby is born, it is placed in a plastic bag up to the baby’s neck.
There once was a time when the scene might have ended differently. Today, placing a premature baby in a warming bag is a common delivery room practice, a move that prevents a preemie’s body temperature from dropping and lowers the baby’s chances of complications and death.
Robin Dail has seen the correlation between temperature and health outcomes firsthand during her lengthy career as a NICU nurse. “A little tiny premature baby that comes out wet and is then whisked away from the mom over to that warming table — they just freeze in that process,” says Dail, now the Health Sciences Endowed Professor in USC’s College of Nursing. “The staff want to get it breathing, and sometimes they don’t concentrate on keeping the baby warm. That can affect all their body systems.”
So 20 years ago, she conducted a groundbreaking study to prove the bags could effectively reduce hypothermia in preterm infants. As a result, using them is now standard practice worldwide. But Dail continues to seek better health outcomes for infants and their families as director of the university’s new Perinatal, Pediatrics, and Family Research Center.
Launched last fall, the PPFRC brings together interdisciplinary researchers, clinical faculty members and doctoral students to study health issues related to pregnancy and childhood.
The center’s work comes at a critical time. Figures from the Centers for Disease Control show that the nation’s maternal death rate has increased from about 17 deaths per every 100,000 live births in 2018 to nearly 24 per 100,000 in 2020. Black women are three times more likely to die than white women.
And while overall infant mortality rates continue trending downward, the U.S. still saw nearly 20,000 infant deaths in 2021. Significant racial disparities are seen here, too: Black infants are more than twice as likely to die as white ones.
Mothers and children are especially vulnerable in South Carolina, where inadequate prenatal care and high rates of morbidities — conditions such as hypertension, diabetes and renal failure — can cause pregnancy complications. And the state’s high preterm birth rate sets children up for lifelong health challenges, particularly when socioeconomic barriers limit access to early interventions.
“Much of our research is aimed at preventing neurologic developmental delays and other health challenges in children born premature,” Dail says. “We know families experience socioeconomic stress due to complications from prematurity. We aim to decrease that burden on families and, ultimately, society.”
Autism spectrum disorder is another neurodevelopmental disorder first diagnosed in early childhood, and it affects children born premature at a higher rate than the general population. Dail, who studies autonomic nervous system dysfunction in preemies, has teamed up with fellow center member Jessica Bradshaw, a psychology associate professor who studies early autism detection methods in infants. The two hope to gain insight on how their research overlaps.
Even though the center is less than a year old, there are already a multitude of research topics in the pipeline: childhood obesity, childhood asthma, optimizing health for pregnant Black women and improving their breastfeeding rates.
“This represents a huge opportunity for USC,” Dail says. “We are becoming a magnet for researchers in this area, and it’s helping us recruit faculty and grow the national reputation of the university in this area. I think it’s impactful, and I’m extremely proud of the center.”
Expanding access
Patti Fabel, College of Pharmacy
In South Carolina’s most rural counties, seeing a doctor to discuss birth control
options can be a frustrating process. Appointments often need to be scheduled months
out. Patients may need to take time off
work, find transportation and line up child care. And the longer all that takes, the
higher the risk of unplanned pregnancy.
A new law is changing that. Last year, Gov. Henry McMaster signed off on the Pharmacy
Access Act, which allows South Carolina pharmacists to prescribe contraceptives without
a doctor’s prescription. Passed with broad bipartisan support, the bill aims to improve
birth control access statewide, particularly
in rural areas where health care providers are scarce.
But putting legislation into practice involves a lot of legwork. That’s where Patti Fabel comes in. Fabel, an associate professor and executive director of the Kennedy Pharmacy Innovation Center in the College of Pharmacy, is part of the team designing the training for pharmacists and pharmacy students who want to become birth control prescribers. USC’s pharmacy curriculum already includes extensive education on contraceptives, covering everything from medicinal chemistry to contraindications. The new certification training will supplement that by explaining the legal requirements specific to South Carolina.
“We have to talk to patients about Medicaid and enrollment in Medicaid. We have to assess for interpersonal violence and human trafficking,” Fabel says. “And so we’re going to incorporate some of these things that pharmacists aren’t really trained to do on a regular basis.”
And pharmacists are open to participating. A residency research project led by 2022
Pharm.D. alumna Tate Cook Owens surveyed pharmacists across the state to gauge their attitudes about the new legislation
and identify potential barriers. While hesitancy was an issue 17 years ago when the
FDA approved over-
the-counter sales of Plan B, concerns now focus mainly on implementation logistics.
“The biggest hurdles were mainly about their staffing concerns, the time that they had to devote to this service and making sure that they were given the resources needed to do it appropriately. That’s fixable,” Fabel says.
Patients still need to see their doctors for routine preventive care, such as cancer screenings. But those screenings are no longer a prerequisite to accessing birth control, meaning women have more freedom when choosing how to prevent unplanned pregnancies. That could translate into lower maternal morbidity and mortality rates.
“An adult female can decide she needs hormonal contraceptives without a physician,” Fabel says. “At that point they just need someone to tell them if it is safe and appropriate for them to have this version or should they have that version? And who’s more well-versed in medication and appropriateness of medication than a pharmacist?”
About half of all states have similar laws on the books. Based on responses in those states, Fabel anticipates that the new law will see the most uptake in areas where it’s needed most.
“If a patient doesn’t really have a problem accessing birth control, they’re probably not going to change the way they’re getting their prescription,” she says. “But in those areas of the state where it’s really tough for them, where it’s going to take them six months just to get an appointment with their OB, and their physician is the type that says that I’m not going to send in refills until you come see me — yeah, those patients are probably going to go to the pharmacist.”
Changing the rural health care landscape
Peiyin Hung, Arnold School of Public Health
Growing up as a first-generation rural-to-urban migrant in Taiwan, Peiyin Hung saw firsthand the challenges rural residents face when accessing health care. Her grandmother, who lived in the Taiwanese countryside, commuted to an urban hospital for specialized care. Before passing away, she explained to Hung the struggles of seeking treatment at a large, crowded medical center.
That experience stayed with Hung when she came to the U.S. for grad school — and it sparked her interest in changing the rural health care landscape.
In 2015, while researching health care access, she was struck by a concerning trend: Almost half of rural U.S. counties lacked any hospital obstetric units, and many were losing these services altogether. At the time, very few people were talking about the issue, she says. Her data suggested they should be.
“I’m looking at this data and thinking, ‘This is not right,’” Hung says. “All these
hospitals are responding with ‘no OB’ or ‘no OB after a certain point.’” The results,
which her team published in 2017, showed that
9 percent of rural counties in the U.S. lost their hospital obstetric services between
2004 and 2014.
Now an assistant professor in USC’s Arnold School of Public Health and deputy director
of the Rural
and Minority Health Research Center, Hung is still investigating rural health disparities
and their impact on maternity care. Maternal morbidity and mortality are critical
areas of study because they can pinpoint shortcomings in maternity care policy and
practice. Severe maternal morbidity affects tens of thousands of Americans annually,
and this prevalence is higher in rural populations.
While the reasons behind the urban vs. rural maternal health disparities remain elusive, Hung has begun connecting the dots.
“Many social determinants of health contribute to these rural and minority maternal disparities; these can have cumulative impacts that persist across generations,” she says. “Structural racism has a ripple effect on maternal health outcomes in rural communities, where health care resources and transportation infrastructure are often limited. For generations, many rural families have been trapped in these under-resourced communities with no way to move to more prosperous or resourceful regions, leading to worse access and outcomes for them and their children.”
Hung and her team have studied the disparities in severe maternal morbidity and mortality rates by Black residential segregation. Their 2022 study found that highly segregated Black communities experience a higher rate of life-threatening complications. The pandemic has exacerbated these disparities for Hispanic women living in highly segregated areas; their rate of morbidities is now nearly twice that of their white counterparts.
In recognition of her pioneering work in maternal health equity, Hung and her multidisciplinary team recently received a $3 million grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to study how telehealth can improve maternal care for rural and racial minority women during the pandemic. Their findings could inform insurance providers and federal policymakers.
“While telehealth appointments can’t replace in-person exams or tests, they offer
an efficient way for patients and providers to communicate about problems before they
become serious health issues,” she says. “Audio-only telehealth appointments, in particular,
show promise for mitigating disparities caused
by the digital divide.”
Hung already has a track record of solving the maternity care crisis in rural and racial minority communities. In 2018, her dissertation informed the passage of the Improving Access to Maternity Care Act, which requires the Health Resources and Services Administration to identify areas with shortages of maternity care providers.
“This is my passion — to solve health disparity issues and inform policymakers and decision makers for necessary actions,” she says. “I hope to inspire my students to join this mission, and they can carry the torch and continue to make an impact on rural families in their own way.”
Addressing birth inequities
Kathryn Luchok, College of Arts and Sciences | Jihong Liu, Arnold School of Public Health
Across the U.S., more than 2 million women of childbearing age live in maternity care deserts — counties without obstetric care facilities and providers. When maternity care is hard to come by, women are less likely to get it. In South Carolina, nearly one in five pregnant women receives inadequate prenatal care, according to the March of Dimes.
“People don’t realize sometimes how rural a state we are, particularly if they live in one of the urban areas, and they don’t really understand how difficult it can be to get the kinds of services that are necessary,” says Kathryn Luchok, a senior instructor in the Department of Women’s and Gender Studies and affiliate faculty member in the Department of Anthropology.
Since joining the South Carolina Birth Outcomes Initiative’s Birth Equity work group 12 years ago, Luchok has helped the organization improve maternal care disparities by supervising student projects aimed at better understanding the issue. Racial disparities in the state’s rural areas have been a particular area of focus.
“When you look at birth equity, rural areas are more predominantly African American and Hispanic, so if you don’t address the needs there, you’re also not addressing the needs for people of color who have less than stellar outcomes in the state to begin with,” Luchok says.
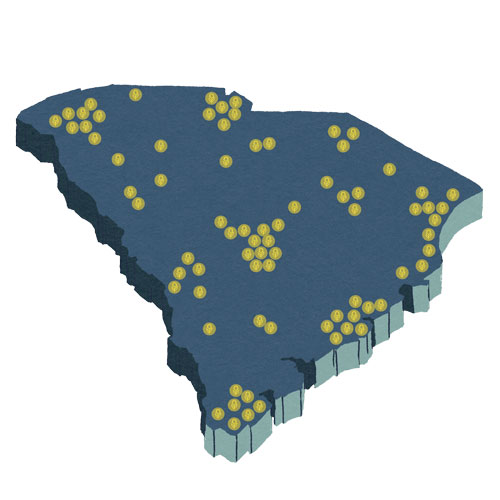
One project that’s garnered attention, a comprehensive map of perinatal services in South Carolina, was created last year by exercise science major and medical humanities minor Taylor Olson for her Honors College senior thesis. Women’s and gender studies major Teddi Meier did some follow-up work on the map for her capstone project.
Built with data from a variety of sources, including provider data from USC’s Institute for Families in Society, the map allows users to search for everything from hospitals to licensed midwives, making it easier for women in rural areas to identify the nearest maternity care provider. Not only is it guiding the Birth Equity work group's objectives, but it has potential to influence how state lawmakers allocate resources.
“We’d like to do quarterly updates and also have a way for providers to be able to tell us their updates, changes or things that they add or delete,” Luchok says. “But in the meantime, we’re using the map to help us figure out where the gaps in services really are.”
Changes in policy and practice are also needed. Another of Luchok’s Honors College students, public health major Zola Jane Aplin, wrote a white paper for her senior thesis to examine what has worked in other states. California, for example, now equips hospitals with emergency response toolkits to treat conditions like hemorrhage and preeclampsia, a move that helped reduce the state’s maternal mortality rate by 55 percent from 2006 to 2013, despite rising rates across the country during the same time period.
Federally funded Healthy Start programs have also helped move the needle, Luchok says. Healthy Start focuses on communities with high infant mortality rates and offers a range of services to improve outcomes before, during and after pregnancy. A study led by Arnold School of Public Health epidemiology professor Jihong Liu earlier this year found that Midlands Healthy Start participants experienced improved prenatal care, breastfeeding initiation and supplemental nutrition program participation.
“We already know what we need to do, but we need the political will and the dollars to go to these kinds of programs and to look very holistically and multidimensionally about the way we address these issues,” Luchok says. “One thing will not change it. It has to be all these things in concert, and you have to look at where people are coming from and how they’re interfacing — from well before they got pregnant, through their pregnancy, through their delivery and into the postpartum.”
Implementing social-emotional learning strategies
Aidyn Iachini, College of Social Work | Kate Ascetta, Robbie Ross and Shelly Curcio, College of Education
Reading. Writing. Arithmetic. And maybe an end-of-the-day reflection on how students have demonstrated kindness.

Today’s K-12 curriculum goes beyond the three R’s to include social-emotional learning, an educational method that has become commonplace in schools over the past two decades. SEL hinges on the idea that social and emotional skills carry just as much weight as math, science or reading when it comes to success in the classroom and in life.
There’s ample evidence it works. Studies have demonstrated improved outcomes in a number of areas, including math and literacy scores, high school graduation rates and childhood obesity. After the pandemic disrupted how children learn and socialize, educators have expressed an even greater need for comprehensive SEL interventions and programming.
“For a period of time, kids were learning through computer screens,” says Aidyn Iachini, an associate professor in the College of Social Work. “The need for SEL was always there, but after COVID, many of these needs have been exacerbated.”
So last year, Iachini and College of Education colleagues Kate Ascetta, Robbie Ross and Shelly Curcio conducted an ASPIRE-funded study to design an intervention framework for helping
schools choose
and plan to implement the SEL programs that work best for their students.
“We know a lot of schools will say, ‘We use this program, and we’ve been using it for 10 years,’” Iachini says. “But we also know that the needs of students are constantly changing. This grant helped us work towards building the capacity and the readiness of schools to use their own data to guide decision-making around social-emotional learning programs and practices.”
The study, “ReadySET: School Readiness for Teaching Social-Emotional Learning Skills,” targeted teachers, school mental health professionals and administrators in two South Carolina elementary schools, with a focus on kindergarten through third grade. Survey data was collected from the participants over the course of the study, and that data was compiled into several school-based reports that guided the intervention. The researchers also developed and shared modules, PowerPoints, toolkits and other resources.
“Big picture, these schools gained some new information through that process in terms of what their needs are, what their programs are targeting and whether those things match up,” Iachini says.
That information will help schools decide if it’s time to try something different, and according to Iachini, the process has potential to be replicated beyond South Carolina. “It will translate nicely, I think, into multiple districts and school contexts across the U.S.,” she says, “because it’s asking schools to use their own data to figure out which SEL programs are best for their particular needs.