Vedantam, P., Tzeng, T. R. J., Brown, A. K., Podila, R., Rao, A., & Staley, K. (2012). Binding of Escherichia coli to functionalized gold nanoparticles. Plasmonics, 7, 301-308.
Callahan, C. T., Wilson, K. M., & Ely, B. (2016). Characterization of the proteins
associated with Caulobacter crescentus bacteriophage CbK particles. Current microbiology, 72, 75-80.
Scott, D. C., Scott, L., Wilson, K., Ross, K., Ingram, D., Lewter, T., ... & Ely, B. (2018). Complete genome sequence
of a wild-type isolate of Caulobacter vibrioides strain CB2. Microbiology resource announcements, 7(17), 10-1128.
Wilson, K., & Ely, B. (2019). Analyses of four new Caulobacter Phicbkviruses indicate independent
lineages. The Journal of General Virology, 100(2), 321.
Ely, B., Wilson, K., Ross, K., Ingram, D., Lewter, T., Herring, J., ... & Scott, D. (2019). Genome comparisons
of wild isolates of Caulobacter crescentus reveal rates of inversion and horizontal
gene transfer. Current microbiology, 76, 159-167.
Wilson, K. M., Miranda, K., Kaul, M., Nagarkatti, P. S., & Nagarkatti, M. (2020). Single cell
profiling illustrates down-regulation of GM42031 in macrophages and microglia as a
potential mechanism of neuroinflammation in transgenic GFAP-gp120 mice. The Journal of Immunology, 204(1_Supplement), 225-12.
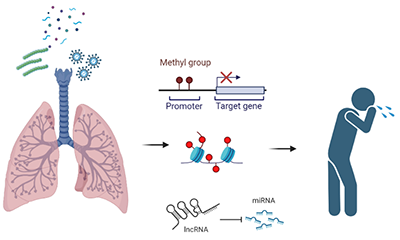
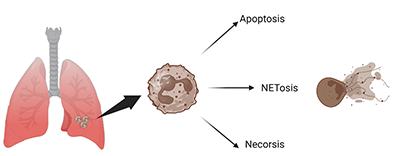
Mohammed, A., FK Alghetaa, H., Miranda, K., Wilson, K., P. Singh, N., Cai, G., ... & Nagarkatti, M. (2020). Δ9-tetrahydrocannabinol prevents
mortality from acute respiratory distress syndrome through the induction of apoptosis
in immune cells, leading to cytokine storm suppression. International Journal of Molecular Sciences, 21(17), 6244.
Wilson, K., Zhu, F., Zheng, R., Chen, S., & Ely, B. (2020). Identification of proteins associated
with two diverse Caulobacter phicbkvirus particles. Archives of virology, 165, 1995-2002.
Becker, W., Alrafas, H. R., Wilson, K., Miranda, K., Culpepper, C., Chatzistamou, I., ... & Nagarkatti, P. S. (2020). Activation
of cannabinoid receptor 2 prevents colitis-associated colon cancer through myeloid
cell de-activation upstream of IL-22 production. Iscience, 23(9).
Ely, B., Liese, J., Corley, S., Nguyen, D., Wilson, K., & Berrios, L. (2020). Novel Caulobacter bacteriophages illustrate the diversity of
the podovirus genus Rauchvirus. Archives of virology, 165, 2549-2554.
Wilson, K. M., Cannon, A. S., Sultan, M., Nagarkatti, P., & Nagarkatti, M. (2021). A single-cell
atlas of the lung mononuclear cell response in Staphylococcus Enterotoxin B-induced
Acute Respiratory Distress Syndrome. The Journal of Immunology, 206(1_Supplement), 110-15.
Becker, W., Alrafas, H. R., Busbee, P. B., Walla, M. D., Wilson, K., Miranda, K., ... & Nagarkatti, P. S. (2021). Cannabinoid receptor activation on
haematopoietic cells and enterocytes protects against colitis. Journal of Crohn's and Colitis, 15(6), 1032-1048.
Dopkins, N., Miranda, K., Wilson, K., Holloman, B. L., Nagarkatti, P., & Nagarkatti, M. (2021). Effects of orally administered
cannabidiol on neuroinflammation and intestinal inflammation in the attenuation of
experimental autoimmune encephalomyelitis. Journal of Neuroimmune Pharmacology, 1-18.
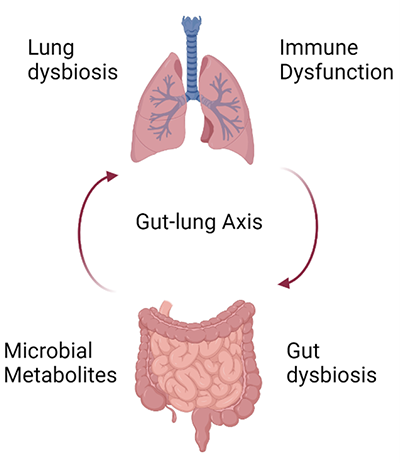
Sultan, M., Wilson, K., Abdulla, O. A., Busbee, P. B., Hall, A., Carter, T., ... & Nagarkatti, M. (2021).
Endocannabinoid anandamide attenuates acute respiratory distress syndrome through
modulation of microbiome in the gut-lung axis. Cells, 10(12), 3305.
Cannon, A. S., Holloman, B. L., Wilson, K., Miranda, K., Dopkins, N., Nagarkatti, P., & Nagarkatti, M. (2022). AhR Activation
Leads to Attenuation of Murine Autoimmune Hepatitis: Single-Cell RNA-Seq Analysis
Reveals Unique Immune Cell Phenotypes and Gene Expression Changes in the Liver. Frontiers in Immunology, 13, 899609.
Wilson, K., Nagarkatti, M., & Nagarkatti, P. (2023). CBD Treatment Improves Fatal Inflammatory
Response Exhibited in SEB-Induced ARDS. Journal of Biological Chemistry, S172-S172.
Alghetaa, H., Mohammed, A., Singh, N., Wilson, K., Cai, G., Putluri, N., ... & Nagarkatti, P. (2023). Resveratrol attenuates staphylococcal
enterotoxin B-activated immune cell metabolism via upregulation of miR-100 and suppression
of mTOR signaling pathway. Frontiers in Pharmacology, 14, 1106733.
Holloman, B. L., Cannon, A., Wilson, K., Nagarkatti, P., & Nagarkatti, M. (2023). Aryl hydrocarbon receptor activation ameliorates
acute respiratory distress syndrome through regulation of Th17 and Th22 cells in the
lungs. MBio, 14(2), e03137-22.
Holloman, B. L., Cannon, A., Wilson, K., Singh, N., Nagarkatti, M., & Nagarkatti, P. (2023). Characterization of Chemotaxis-Associated
Gene Dysregulation in Myeloid Cell Populations in the Lungs during Lipopolysaccharide-Mediated
Acute Lung Injury. The Journal of Immunology, 210(12), 2016-2028.